From My 2023 Recovery from Surgery to My 2024 Chest Pain Journey to Recovery Again
After writing my last three HCM recovery blog posts (WKYC TV-3, Spectrum News 1, UH patient story), I did not expect to ever write about my heart condition again. Since hypertrophic cardiomyopathy (HCM) is a progressive heart condition, I did think in the back of my mind that I may need additional treatment that I might write about at some point in my life, but I assumed that it would be in the distant future or maybe never happen within my remaining lifetime. (For background, and to learn about HCM, please see my first HTM blog post: My Hypertrophic Cardiomyopathy Part One: Diagnosis & Medication)
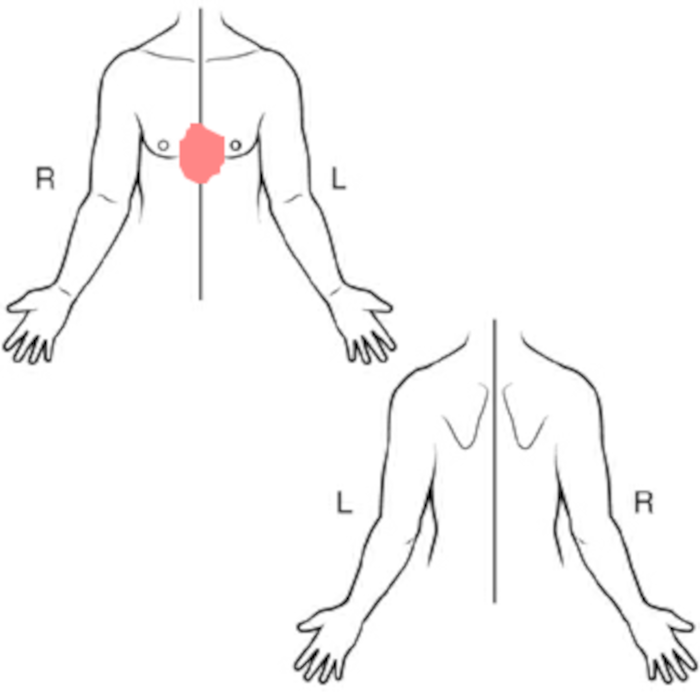
At first, I debated listing this as my seventh HCM blog post, since at the time I write this, my current chest pain and occasional breathlessness has been confirmed to not be caused by my ongoing HCM cardiac condition. As you read this HCM blog post, you will learn how my chest pain does, most likely, relate to my April 27, 2023, open-heart surgery, which I needed due to having HCM (Learn about my surgery in the blog post: My Hypertrophic Cardiomyopathy Part Two: Surgery). I write "most likely," since I write this while still in the middle of actively seeking treatment that will be successful in stopping my chest pain.
I want to be clear that my chest pain is mild most of the time, but it has worsened the last two months (July/August 2024), and is now interfering with all of my normal life activities. My chest pain is difficult to treat, since it grows and subsides in intensity seemly randomly -- nothing makes it worse and nothing makes it better.
I decided to write the majority of this blog post starting in mid-August 2024 . . .
to capture the current status of my progress to find a successful treatment while it is still happening.
since I find that writing is something that I can do while in pain/discomfort, and it helps distract me from my current situation.
as part of my goal to help me accept what I don't have control over. (This is hard for me.) Documenting the treatment process helps me mentally.
to, most importantly, have a positive outlook for the future. Notice that the title includes the word "Recovery" at a time when there is no guarantee that I will get better. My plan is to write about what is happening to me through the end of August 2024, and then later add the final outcome which I expect to be positive!
If you are reading this seventh HCM blog post, it means that I published it because the journey that I document in the following text ended in the success I desired. To all those people that I mention in this blog post, I am grateful for their part in helping me to leave my chest pain in the past and now enjoy my life fully again!
December 2023 & January 2024 - Big Plans for the New Year!
After having illness and open-heart surgery consume the first half of 2023, I started the first days of 2024 by sharing the following on social media to a fellow blogger:
... so the adventure begins.
. . .
I have big plans for 2024, and I hope a year from now we both can report we had great times in 2024.
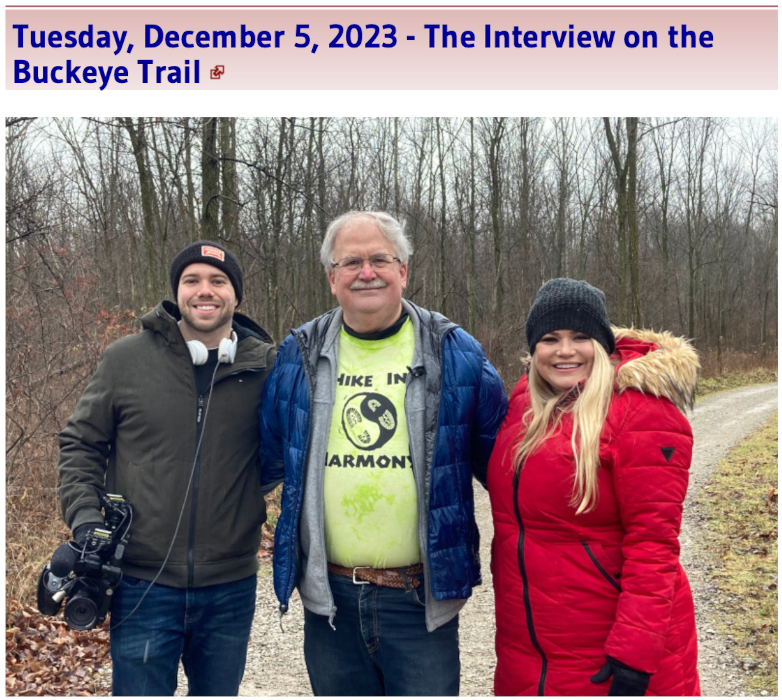
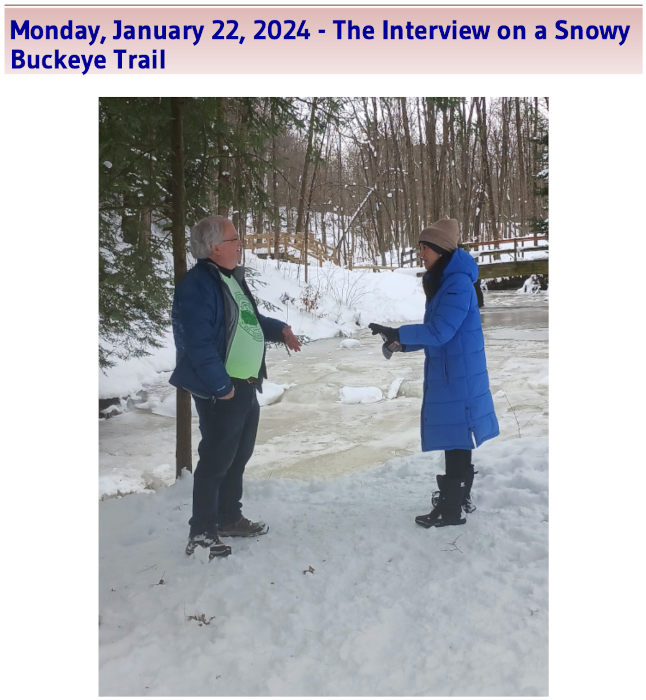
I had good reason to expect 2024 would not only be a busy year, but also a year containing some real adventure. I ended 2023 preparing for the new year by making plans for two big trips in 2024, and also by joining a gym that in the new year I continued to visit three to five days a week. I also had reason to feel positive as we entered 2024 because my post-surgery adventure story had been first broadcast by WKYC TV-3 on December 12, 2023, and then I was interviewed for another story on January 22, 2024, by a Spectrum News 1 reporter:
Blog Date: December 28, 2023 - My HCM Part Four: Recovery & A.T. Hike Featured on WKYC TV-3
Blog Date: February 15, 2024 - My HCM Part Five - Recovery: A Snowy Interview with Spectrum News 1
"Saturday, February 10, 2024 - Spectrum News 1 Shared My Story for American Heart Month"
I was told that my 2023 backpacking trip was unique, since I was able to take it just five months after my surgery. While it was a great, enjoyable adventure, it was also for me a very successful test to see if I could do a much longer backpacking trip in 2024.
While preparing this blog post, I found the following in my cardiologist Eiran Gorodeski's notes from when I met with him on December 15, 2023. I had some chest discomfort, but I thought it just related to some normal stress in my life taking care of a family member. I assumed that the pain was just due to stress, and not heart related. The chest discomfort did not interfere in any of my activities, so I assumed that it would end on its own. I did not know that it was the first indication of a problem that would interfere with my life seven months later:
[Friday, December 15, 2023, 8:40 am] Progress Notes Written by Eiran Gorodeski Advanced Heart Failure and Cardiac Transplantation Cardiology Stuart O Smith Jr. . . . Had some symptoms of heaviness in chest this past weekend, in setting of stress related to a family member's health condition. ... Pin point tenderness to left of sternum on palpation ... Written by Nurse . . . Denies fatigue, shortness of breath, dyspnea on exertion, orthopnea, ... Patient reports chest pain. He states he was in cardiac rehab and then joined [gym]. He does not get chest pain when exercising, but he believes it is stress related. He states it feels like a "heaviness" and lasts approximately 30 minutes . . . Over the last week, he has experienced a couple seconds of "fluttering" in his chest.
Since I felt fully recovered from my HCM symptoms and heart surgery during the second half of 2023 and this first month of 2024, I wanted to now make up for time lost in 2023 by being even more active. I looked forward to continuing my normal life!
Mid-February 2024 - Chest Pain Now Noticeable
By mid-February, my chest pain started to becomes more noticeable, but most of the time, it was not interfering with my normal activities. For example, you can read in my blog post how I started off the month strong by completing the Cleveland Metroparks 2024 Trail Challenge in five days. I also worked out at a gym on four mornings, and ended the week by attending a challenging Northeastern Ohio Orienteering Club event. Then, two weeks later, Monday, February 19, 2024, through Friday, February 23, 2024, I skipped going to the gym, since my heart hurt (chest heavy). Then, strangely enough, the next day (Saturday, February 24, 2024), I felt fine enough to go outside in the bitter cold dancing into the night at the Brite Winter festival. See these two blog posts for more details:
I wanted to list these two outdoor activities to start this blog post about pain to show what my life was like before my symptoms got worse. Please go to sosAssociates.com/Blog to read what I wrote about more events I attended during the first half of 2024.
Wednesday, February 28, 2024, is Hypertrophic Cardiomyopathy Awareness Day
In addition to the February 10, 2024, Spectrum News 1 American Heart Month story about me that I mentioned above, I was asked by the University Hospitals Harrington Heart & Vascular Institute Senior Media Relations Strategist to have my story added to The Science of Health blog and the Heart & Vascular Patient Stories sections of the University Hospitals website for February -- American Heart Month.
I provided the photo for the story, and approved the story before it was published on the hospital's website. You can read my blog post and the original post here:
HCM Patient Returns to Hiking the Appalachian Trail
February 5, 2024
I chose to publish my blog post about the University Hospitals story about me on Wednesday, February 28, 2024, since it was Hypertrophic Cardiomyopathy Awareness Day 2024. My wife and co-blogger, Julie, and I also watched the University Hospitals webinar presented on that day. I decided to include the HCM Day University Hospitals webinar in this blog post, since I want to highly recommend watching it to learn about this common heart condition. (I also added it as a comment to my 2024 HCM Awareness Day blog post.)
FYI, as part of my treatment in 2023 and now in 2024, I have met in person with all but one of the healthcare providers that were featured in this webinar:
Hypertrophic Cardiomyopathy (HCM) – The Most Common Inherited Heart Condition
February 28, 2024
By Judith Mackall, MD, Michael Zacharias, DO, Eiran Gorodeski, MD, MPH, Bradley Lander, MD, and Diane Donato, RNHypertrophic Cardiomyopathy (HCM): The Most Common Inherited Heart Condition
University Hospitals
. . . Feb 29, 2024
Hypertrophic cardiomyopathy (HCM) is the most common inherited heart condition, affecting about one in 500 people. However, up to 85% of individuals living with the disease don’t know they have it and remain undiagnosed. HCM causes abnormal thickening of the main pumping chamber of the heart, impacting heart function and rhythm. Many individuals with HCM can lead normal lives, but over time, untreated or undiagnosed HCM can lead to a stroke, atrial fibrillation, heart failure or sudden cardiac death. HCM is highly complex and can also be passed on to other family members. The Hypertrophic Cardiomyopathy Center team of University Hospitals Harrington Heart & Vascular Institute provides an overview of HCM, including treatment options and exercise recommendations. For more information about HCM care, visit https://www.uhhospitals.org/services/heart-and-vascular-services/conditions-and-treatments/cardiomyopathy/hypertrophic-cardiomyopathy
00:00 Start
01:26 What is an Inherited Heart Condition?
04:33 What is Hypertrophic Cardiomyopathy?
12:33 HCM Treatment Options: Medications, Catheter-Based and Surgical Therapies
25:54 Heart Rhythms and HCM: Atrial Fibrillation and Sudden Cardiac Death
40:24 Is It Safe to Exercise with Hypertrophic Cardiomyopathy?
48:40 Navigating the HCM Care Process
March & April 2024 - Testing Hypothesis 1: Chest Discomfort Caused by HCM or Related Cardiac Condition
Since Hypertrophic Cardiomyopathy (HCM) is a progressive, genetic heart disease that I will always have, it was logical to first test if my chest pain/discomfort that I was experiencing in 2024 was caused by my cardiac condition. The following sections outline what steps were taken in March and April 2024, to test if my heart was the issue causing my chest pain.
Tracking Chest Pain Issues
I was instructed by the University Hospitals Hypertrophic Cardiomyopathy (HCM) Center Team to keep a personal journal tracking my chest pain and related health issues. From March 9, 2024, through April 23, 2024, I tracked having some type of chest pain or discomfort every day except for one. While this daily issue was worse than in January/February, I still maintained my normal lifestyle during this time period.
I stopped tracking on Wednesday, April 24,2024, since it was too discouraging to see pain listed every day, plus I had an appointment with my cardiologist the next week (I emailed Dr. Gorodeski a copy of the tracking file). I also completely stopped going to the gym on April 24, 2024, since it was suggested that I might need more rest to let whatever was hurting my chest heal.
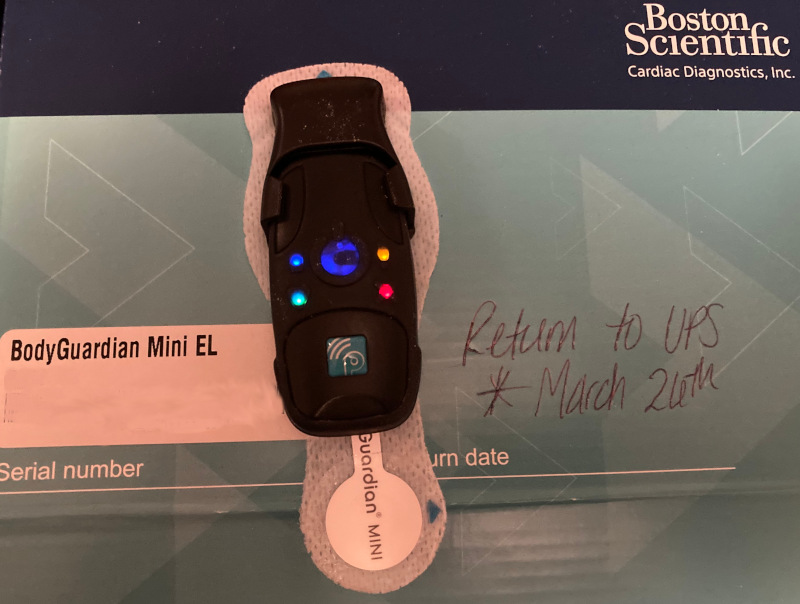
Holter monitor
[Monday, March 11, 2024] Telephone Encounter
Written by Nurse Diane D
Dr. Gorodeski would like patient to wear a holter monitor to assess for arrhythmias. Will await results of holter to determine next steps or need for additional testing.
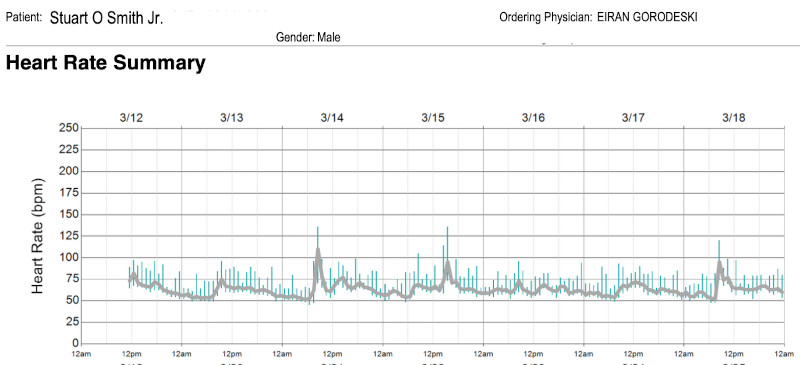
I did a long-term Holter study (March 12-26) and received the very good results on April 4, 2024.
[Tuesday April 2, 2024] Telephone Encounter Written by Nurse Diane D Patient continues to experience occasional episodes of chest heaviness & breathlessness. It is not associated with physical activity or exertion; however symptoms are reminiscent of pre- myectomy symptoms. State lungs feel heavy at times. Reviewed with Dr. Gorodeski. In addition to his holter monitor (current) & scheduled echocardiogram, Dr. Gordoeski would like a CXR, CBC, BNP & BMP drawn. Patient aware & verbalizes understanding.
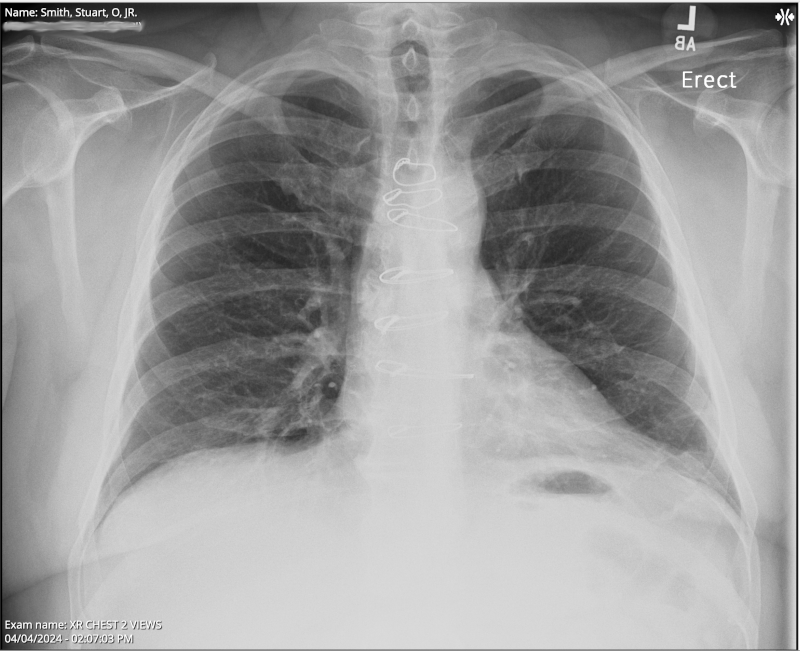
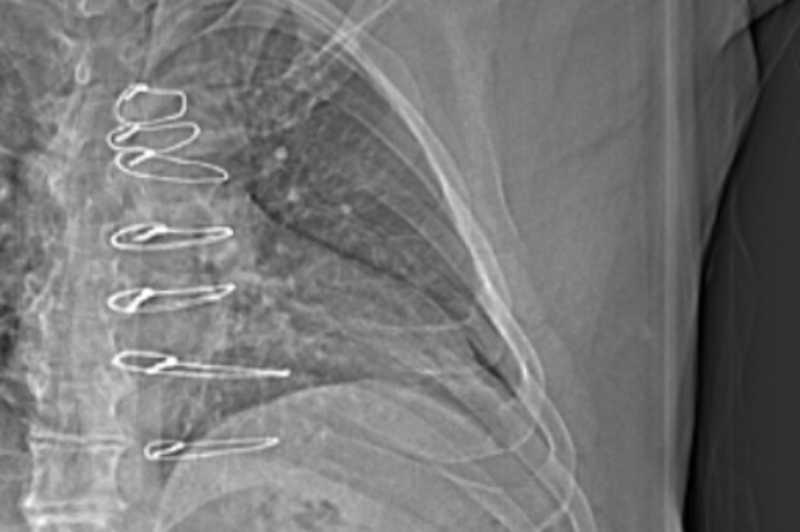
Chest X-ray
XR Chest 2 view Collected on April 5, 2024 7:42 PM . . . Impression 1. No evidence of acute cardiopulmonary process. . . . ORDERING CLINICIAN: EIRAN GORODESKI FINDINGS: Median sternotomy wires present. CARDIOMEDIASTINAL SILHOUETTE: Cardiomediastinal silhouette is normal in size and configuration. LUNGS: Lungs are clear. ABDOMEN: No remarkable upper abdominal findings. BONES: No acute osseous changes.
The results from my April 4, 2024, chest x-ray looked good. I still find it strange to view my x-rays and see some of the hardware that was left inside me after my April 27, 2023, septal myectomy (open-heart surgery) for Hypertrophic Cardiomyopathy. The notes above mention "Median sternotomy wires present," plus I also have retained epicardial pacing wires left inside me, which I have seen in other x-rays.
To learn more about these wires left in my body in my blog posts:
Please see in my HCM surgery blog post the How is Chest closed after Bypass / Open Heart Surgery age-restricted video (warning some find this graphic video disturbing) that shows how median sternotomy wires were used to close the chest after the surgery.
If you look very closely at the x-ray photo at the top of this blog post, and the following two x-ray photos, you can see the sternotomy wires:
Echocardiogram
(Above are images/videos from my April 5, 2024, echocardiogram.)
4/5/2024 11:20 AM UH Cleveland Minoff Health Center 216-831-834
Today's Visit
You were seen on Friday April 5, 2024.
The following issues were addressed: Hypertrophic cardiomyopathy and Palpitations.
Done Today
Transthoracic echo (TTE) complete for Hypertrophic cardiomyopathy, Palpitations
. . .
CONCLUSIONS:
1. Left ventricular systolic function is normal with a 70% estimated ejection fraction.
2. Spectral Doppler shows a pseudonormal pattern of left ventricular diastolic filling.
3. The patient is post myectomy. There is mild basal anteroseptal thickening (1.3 cm).
4. There is a mild left ventricular outflow tract obstruction (19 mmHg), which is unchanged when compared with prior study from 4/2023.
The results of my April 5, 2024, echocardiogram were very good. For me, the most important item is the "left ventricular outflow tract obstruction (19 mmHg)." See the following quote from my My Hypertrophic Cardiomyopathy Part One: Diagnosis & Medication blog post to understand why 19 is a great number for me a year after my septal myectomy surgery!!!
I am very grateful for having had the opportunity a year ago to have my surgery performed by Dr. Yasir Abu-Omar, the Surgical Director of the Advanced Heart Failure & Transplant Center at University Hospitals Harrington Heart & Vascular Institute.
May 1, 2024, Dr. Eiran Z Gorodeski Appointment
Disproved Hypothesis that Chest Discomfort Caused by HCM or Related Cardiac Condition
[Wednesday, May 1, 2024, 10:00 am] Progress Notes Written by Eiran Gorodeski Advanced Heart Failure and Cardiac Transplantation Cardiology . . . He had cardiac surgery (myectomy) a year ago. He is here now because since February 2024 he developed intermittent pain in mid chest. It is of varying qualities, including sharp at times. It is not related to exercise, and in fact sometimes feels better in the middle/after exercise. He had an evaluation including echocardiogram, chest xray, holter, and blood work. . . . Assessment: Chest wall pain, related to prior surgery. Unclear to me what triggered it several weeks ago, but possibly some injury leading to a flare up.
From my notes from when I met with Dr. Eiran Z Gorodeski on May 1, 2024: He diagnosed me with chest wall pain. (I started with daily chest issues before 2/19/24.) The chest pain is probably as a result of scar tissue, trauma, and wires in my chest. The pain is not cardiac related.
Therefore, after all the tests I had in March and April 2024, we disproved the hypothesis that my chest discomfort was caused by HCM or a related cardiac condition. I entered the new month with very good news -- my chest pain is not cardiac related.
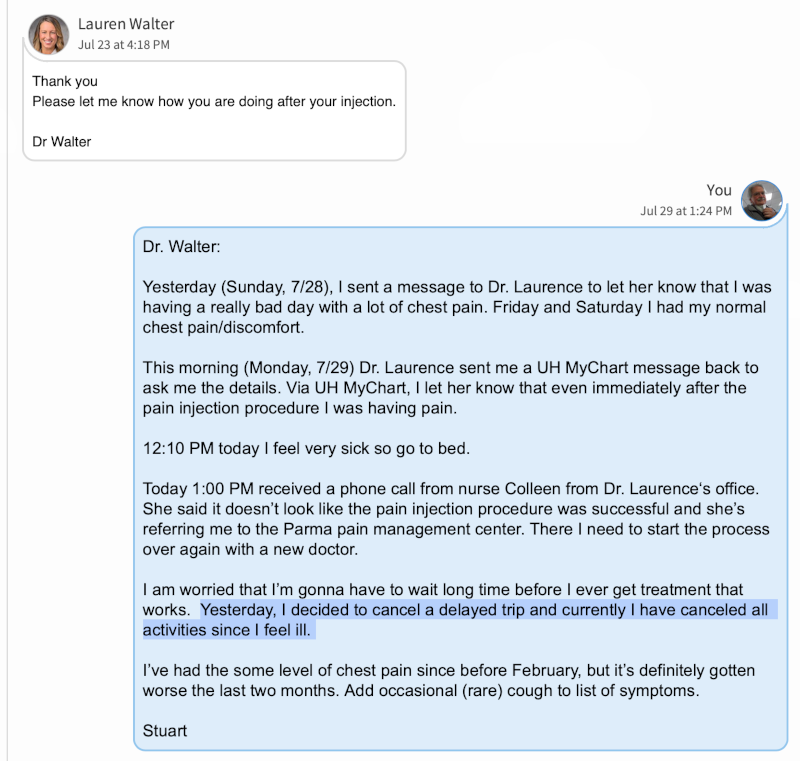
I felt like I was very prepared for my appointment the next day, that I had already lined up with my primary care physician, Dr. Lauren M Walter.
Hypothesis 1 (Cardiac Condition) Rejected
May - June 2024 - Testing Hypothesis 2: Chest Discomfort and Occasional Shortness Of Breath is Caused by Inflammation
Since, on May 1st, it was confirmed that I did not have a cardiac condition, the next day, I started trying treatment options for possible inflammation with Dr. Lauren M. Walter. The following sections outline what steps were taken in May and June, to test if an inflammation in the chest area was the issue causing my pain, before then taking it to the next level in July 2024.
Topical Treatments for Inflammation
[Thursday, May 2, 2024, 8:00 am, Dr. Lauren Walter. Screening for cardiovascular condition.] Progress Notes . . . Stuart O Smith Jr. . . . PMH of HOCM s/p open heart surgery w/ myectomy in April 27, 2023, . . . Patient complaining of chest pain since January. Substernal, nothing seems to cause it and it occurs randomly. It comes and goes, describes it as a heaviness or discomfort. There are episodes when the pain is severe to cause SOB [Shortness Of Breath] on exertion. Not tender to palpation. . . . Motrin does not help with pain.
After my May 2, 2024, appointment, Dr. Walter first had me try topical treatments -- lidocaine (Lidoderm) patches and then diclofenac gel -- but they did not stop the pain.
Oral Medication Treatments for Inflammation
[Thursday, June, 6, 2024, 8:00 am] Progress Notes
Written by Lauren Walter
. . .
Chief Complaint
Patient presents with
• Follow-up
Follow up, has chest pain still
. . .
Stuart O Smith Jr. . . . chest wall pain that comes and goes.
There are not exacerbating or remitting factors that the patient can point to.
Cardiology has stated that this is not cardiac in nature.
The patient also admits to SOB [Shortness Of Breath] that has recently started that goes along with the pain.
The patient has h/o of open heart surgery. He did start an exercise regimen that include weight lifting.
He has tried lidocaine patches and diclofenac gel without relief.
He is scheduled with pain management in July.
He has an Alaskan cruise coming up soon and a large trip in August that he would like to feel better before traveling.
He is very down about the way he is feeling.
. . .
SOB (shortness of breath) - Primary
Relevant Orders
Complete Pulmonary Function Test (Spirometry/DLCO/Lung Volumes)
CT angio chest for pulmonary embolism
A month later, on Thursday, June 6, 2024, I had a follow-up appointment with Dr. Lauren M Walter, where she prescribed three new oral medications. Unfortunately, side effects prevented effective treatment with two of the medications, and after an extended time using a high dose of acetaminophen (Tylenol Extra Strength), I stopped since it did nothing to stop the pain.
Hypothesis 2 (Inflammation) Needs Additional Study
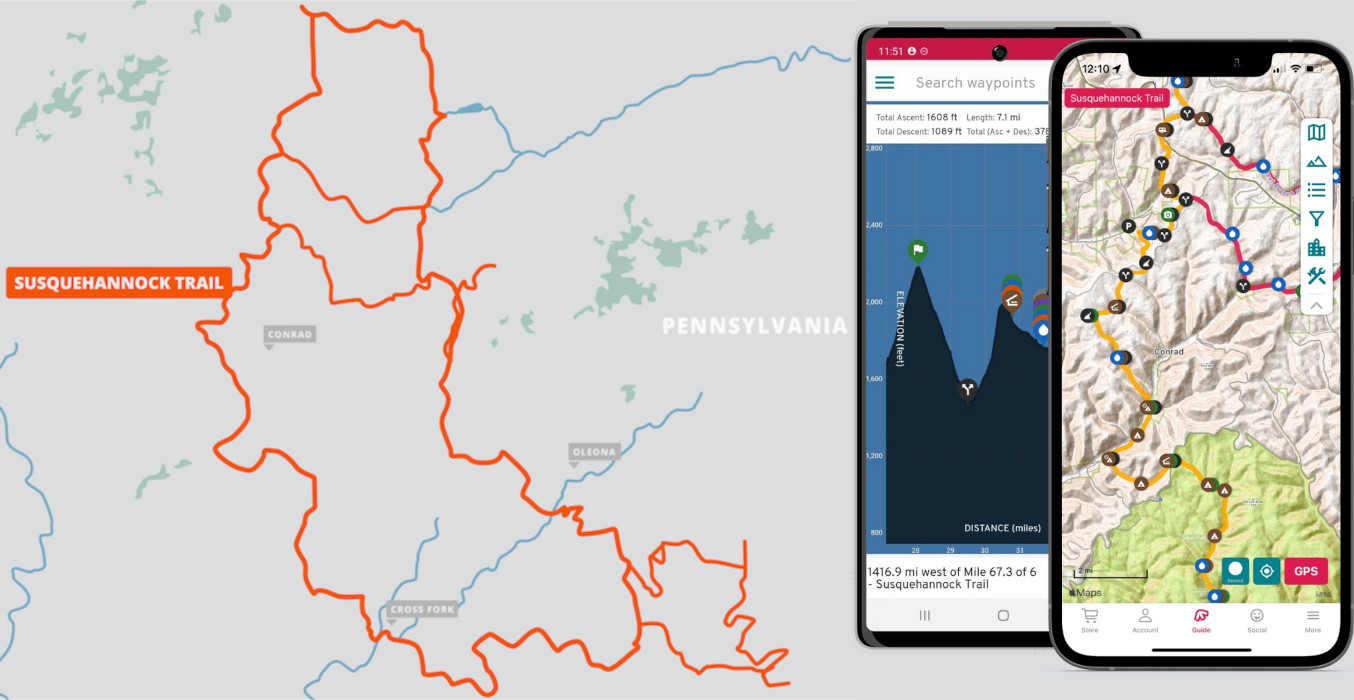
Monday-Wednesday, May 13-15, 2024 - Testing Hypothesis 3: I Can Ignore Chest Discomfort and Backpack for Over a Week
In mid-May, my chest discomfort was not yet preventing me from participating in my normal life activities. I decided the best way to see if I could backpack was to just do it!
The results were mixed. The first and third days, I felt fine. The second day, I just did not feel right, and I leaned toward caution by taking one of the optional shorter loops. I had a great time on my three-day trip, but determined that a longer backpacking trip would not be possible in comfort in my current health situation.
Considering my history of having open-heart surgery a year ago, I found it humorous that one of the hills on the Susquehannock Trail System is described with the following: "STS begins a steep ascent affectionately nicknamed 'Cardiac Climb.'"
Hypothesis 3 (Backpack for a Week) Rejected
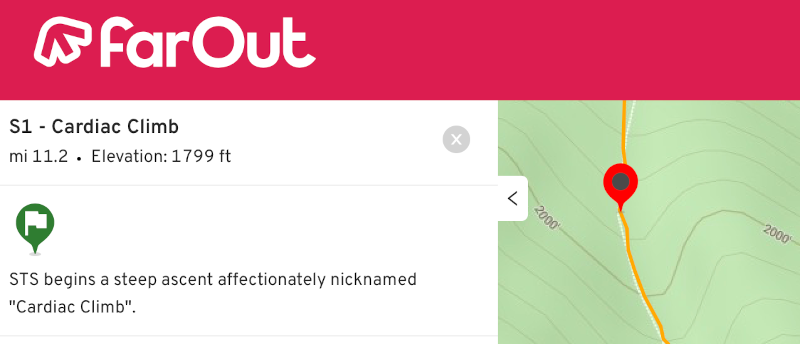
June 2024 - Testing Hypothesis 4: Occasional Shortness Of Breath Caused by Lung Issues
(Pulmonary Function Test & CAT Scan)
By May 2024, a new symptom, that while still mild and only occasional, had become noticeable -- shortness of breath. Dr. Walter arranged for me to have both a Complete Pulmonary Function Test (June 12, 2024) and a CT (computed tomography scan) scan (June 6, 2024) to check for a pulmonary embolism(s). (An embolism is an obstruction of an artery.)
The results of both pulmonary tests were very postive, as I expected. I never really entertained the hypothesis that the issues I had been having were caused by a problem with my lungs.
Hypothesis 4 (Pulmonary Issues) Rejected
End of June - Delayed Next Treatment Step - Travel on Alaska Cruisetour
Dr. Walter wrote in her June 6, 2024, progress notes ". . . an Alaskan cruise coming up soon . . ." The next step in treatment was delayed so that my wife and co-blogger, Julie, and I could go on the Alaskan trip (June 23, 2024 - July 5, 2024) that we have wanted to take for years! We wrote in our Alaska! blog post:
We had everything planned to go to Alaska in the summer of 2023, but decided to postpone our trip until 2024 due to the uncertainty about the recovery time after Stuart's planned open-heart surgery on April 27, 2023 (see HCM part 2: Surgery blog post for details). Our concerns about post surgery recovery time ended up being unfounded, since we ended up taking a wonderful 2023 vacation in Michigan with a lot of walking and bike riding (see our Summer Vacation 2023 blog post).
Yes, the concerns about post-surgery recovery in 2023 were completely unfounded -- two months after the surgery, I was hiking on Ohio's Buckeye Trail and had started 36 sessions on exercise machines three days a week at University Hospitals Cardiac Rehabilitation.
In contrast to my 2023 very physically active vacation in Michigan, during the June 2024 Alaska trip:
I avoided taking stairs
I needed to stop to rest when walking the wooden sidewalks of the Alaskan towns visited
I skipped hiking opportunities
I limited my dancing
It was ironic that we canceled the trip after my 2023 surgery, but now in 2024, I was more limited in walking when touring Alaska. I still had a great time, but my chest pain issues did limit me from doing some of the activities in which I normally would partake. The following quote from our Alaska! blog post hints at my being left out of part of exploration activities:
(It is certainly not like me to send my wife into bear country without me!!)
Despite my physical limitations, we did have a fantastic once-in-a-lifetime trip -- I invite you to please read our blog post:
Blog Date: September 2, 2024 - Alaska!

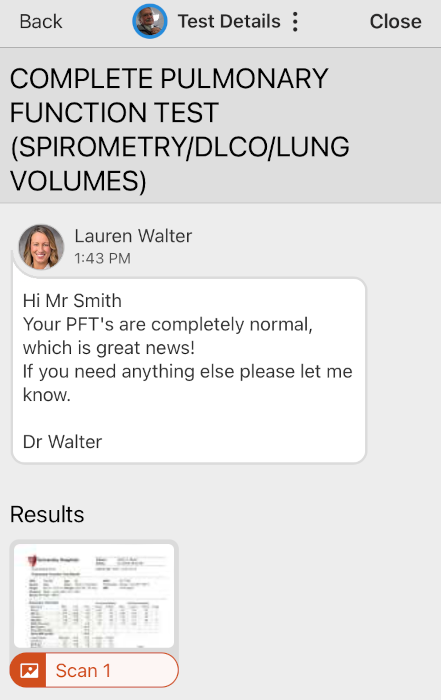
July 2024 - Taking It to the Next Level By Going to University Hospitals Pain Management Services to Further Test Hypothesis 2: Chest Pain is Caused by Inflammation
(Bilateral sternocostal joint injection under ultrasound guidance)
Both my cardiologist, Dr. Gorodeski, and my primary care doctor, Dr. Walter, referred me to University Hospitals Pain Management Services, which was my next step in chest pain treatment after returning from our Alaskas trip.
On July 11, 2024, I was assessed by the Medical Director for Pain Medicine at the University Hospitals Ahuja Medical Center, Melinda Lawrence, MD. She recommended I receive a pain management block, which would be guided by ultrasound into the areas of my chest where pain was present. Dr. Lawrence arranged that she would be the doctor performing the procedure on July 26, 2024. I was very hopeful that this process would work to get rid of the inflammation that I assumed was at the root cause of my chest pain.
The days between the initial assessment date and the procedure date emotionally felt like the longest 15 days of my life. I thought that the placement of medication that would stop the pain, along with a steroid that would facilitate healing, would mean that I would return to my normal life after July 26th.
During the 15 days I was waiting for my pain block injection, I updated the countdown dates that I had in a planning spreadsheet which I used for a big trip that I had scheduled to start on July 22, 2024, to a new start date of August 6, 2024.
The first needle on my right side lower rib area only hurt a little, but the second needle into my left breast tissue did hurt a lot until the numbing agent took effect. After the procedure, a nurse asked me if my chest pain was gone, and approximately 15 minutes after I was in the recovery room, I let her know that I still had my chest pain. The nurse then called in Dr. Adaralegbe, who was assisting with the nerve block procedure, to then meet with me. I had been told before the procedure that it would be a good sign if I had imediate pain relief, but if not, I should wait. Here are the doctor's notes about the procedure:
Reading Physician Reading Date Result Priority Melinda M Lawrence, MD 7/26/2024 Routine Preoperative diagnosis/postoperative diagnosis: Procedure: Bilateral sternocostal joint injection under ultrasound guidance Surgeon: Melinda Lawrence Assistant: Fellow, Adaralegbe Anesthesia: Local Complications: Apparently none . . . history of anterior chest pain just lateral to the sternum. He has reproducible areas of discomfort. We discussed a injection under ultrasound guidance to target these locations. Maximal areas of tenderness identified. There was 1 spot on each side of the sternum, just lateral. . . . Ultrasound was utilized to identify a the most inferior sternal costal joints. Identified first on the left and then right sides. Skin and subcutaneous tissues to the joint was anesthetized using 0.5% lidocaine. A 22-gauge ultrasound needle was inserted and advanced to the appropriate location first on the left and then right sides. Needle was visualized throughout the injection procedure. A total of 3 mL of bupivacaine mixed with 40 mg of methylprednisolone was injected in divided doses among the 2 needles. Needle removed, bandage applied, patient tolerated the procedure well with no immediate complications. Discussed with the patient that he should keep a close eye on how his pain does in the next 1 or 2 hours. If he has immediate relief then that could be a good sign that this is specifically where his pain comes from. It may take a few days for the steroid to set up completely. . . .
As the above doctor's notes indicate, it would have been a good sign if my pain went away soon after the Friday, July 26th procedure. Over the weekend, it became clear that the procedure did not work, and that my chest pain was not caused by inflammation as expected!!
On Sunday, July 28, 2024, I made the painful decision to cancel my big fall trip that I had recently rescheduled to August 6, 2024. ![]() I had been planning the trip since Friday, October 13, 2023, which was the week after returning from my backpacking trip that ended up being featured on the University Hospitals website for American Heart Month 2024.
I had been planning the trip since Friday, October 13, 2023, which was the week after returning from my backpacking trip that ended up being featured on the University Hospitals website for American Heart Month 2024.
Then, on Monday, July 29, 2024, Dr. Lawrence made a referral to the University Hospitals Parma Pain Management Center: 440-743-4333. I really appreciated that Dr. Lawrence and her nurse, Colleen, got back to me so quickly on setting up the next step.
I set up an appointment via the University Hospitals MyChart app, with pain medicine specialist Harpreet Singh, MD, for Wednesday, August 14, 2024. Through Dr. Lawrence's nurse, Colleen, I learned that the next step of my treatment would be trying pain medication that "works on the receptors in the brain by helping decrease pain sensations."
Hypothesis 2 (Inflammation) Rejected
August 2, 2024 - Doctor Asks Me if I Need a Wheelchair
I am taking care of [a family member] since early this morning in the emergency room at Cleveland Clinic Hillcrest Hospital. As I am walking down the hall at the hospital, a Cleveland Clinic doctor sees me and asks if I need a wheelchair. Yes, I must look like a sick person with chest pains to have a doctor who is a stranger ask me if I need assistance.
Just now, I needed to rest a few times walking down the hall since I am not well. It is just mild pain, but it is enough pain to have a stranger see that I am not well.
This year is very different than a year ago — a year ago I felt strong and healthy starting two months after my April 27, 2023, heart surgery. This year I am not well and currently don’t know of treatment options that will succeed.
I’m having a bad month.
Stuart
The text above is a from an email that I sent to a nurse at the University Hospitals Hypertrophic Cardiomyopathy (HCM) Center. It demonstrates how vastly my health has deteriorated this year compared to how I was post-surgery in 2023.
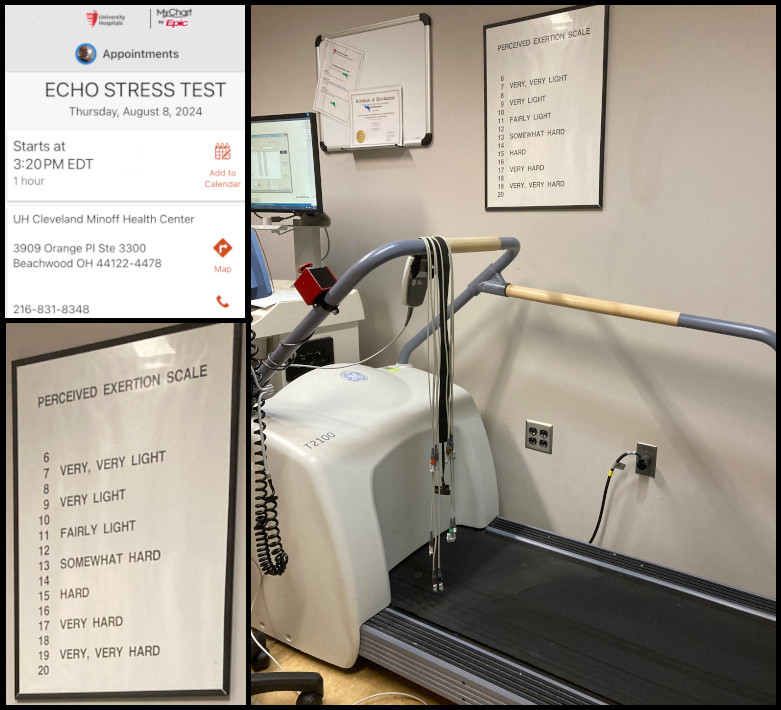
August 8, 2024 - My Echo Stress Test Produced Very Interesting Results!!!
On August 2, 2024, I received a message that Dr. Gorodeski wanted me to have an Echo Stress Test, which he scheduled for August 8, 2024, with Bradley Lander, MD. Unlike the echocardiogram I had back on April 5th, the UH HCM Center required that their HCM patients have a doctor who was a member of the UH HCM Center Team in the room during the stress test -- I was fortunate to have Dr. Lander selected to fill that role.
I was very interested to learn about Dr. Lander's background as the director of the Sports Cardiology Center of University Hospitals Harrington Heart and Vascular Institute. In particular, I was interested in the description of how he ". . . specializes in the care of . . . highly active individuals . . . with hypertrophic cardiomyopathy (HCM)."
Here is part of Dr. Lander's biography which includes a video about his work:
Bradley Lander, MD - Cardiology
University Hospitals
. . . Nov 27, 2023 To schedule an appointment with cardiologist, Dr. Bradley Lander, click here: https://bit.ly/DrBradleyLander
. . .
I had no idea on how I would do on my stress test!!! It is hard to explain how I felt, but I thought I would either not be able to do it at all or that I would do okay on the treadmill. The active symptoms of my chest pain varied sometimes minute by minute, and I knew that I was very out of shape, since I had stopped going to the gym back on on April 24, 2024. In the month of July 2024, I had stopped going to any activities, since my chest pain had interfered with my walking.
The stress test room felt crowded with two nurses constantly checking my vitals and a sonographer operating the echocardiography (cardiac ultrasound) machine. While I was on the treadmill, Dr. Lander and another doctor joined us.
As I started the test, my muscle memory from my experience on a treadmill kicked in and I was able to keep up as they increased the speed of the treadmill. Surprisingly, my chest pain level actually went way down as the stress test proceeded. During the test, I was told to give feedback on how I felt and when I needed to stop, but I never felt like I needed to stop -- I was walking fast and felt good. In the end, I stopped when Dr. Lander told me that he had the information he needed. I felt that I could have continued longer, though it was not at all easy at the fastest speed I obtained. After the stress test, my chest pain returned at a higher level as I rested.
On this day, my body functioned at "above average exercise capacity." Here are some videos of echocardiograms of my heart from the test, followed by some of the results notes:
Exercise Stress Echo
Patient Name: STUART O SMITH Ordering Provider: EIRAN Z GORODESKI
Study Date: 8/8/2024 Reading Physician: Bradley Lander MD
. . .
Study Type: ECHOCARDIOGRAM STRESS TEST
. . .
Patient Performance: The patient exercised to stage III on a Bruce protocol for 9 minutes and 50 seconds, achieving 12.5 METS. . . .
. . .
Summary:
1. The patient exercised for 9:50 on the Bruce protocol, reaching stage 4 and 106% of age predicted maximum heart rate and had above average exercise capacity.
2. Prior to the test the patient had chest pain, which is chronic, rated at 3/10 in severity.
During the test, the chest pain improved, to at best 0.5/10 and the patient reported "it is mostly gone, but it is threatening to come back".
After the protocol was completed and he was laying on the echo table, his chest pain was 5/10 and was sharp in nature.
. . .
3. . . . LVOT gradient at rest is 14 mmHg.
4. There are no stress induced regional wall motion abnormalities. . . .
LVOT gradient post exercise is 20 mmHg. . . .
. . .
Bradley Lander MD
Electronically signed on 8/8/2024 at 3:54:06 PM
On August 8, 2024, I looked at the following websites about how to read my echo stress test results:
Please also note my excellent LVOT gradient levels (rest = 14 mmHg, and post exercise = 20 mmHg) and contrast them to what I had at the April 5, 2024, echocardiogram (19 mmHg), and my pre-open-heart-surgery echocardiogram (56 to 119 mmHg) on December 8, 2022, which led to me being diagnosed with HCM.
On August 10, 2024, I realized that I had previously read and shared on social media an excellent article by Dr. Lander about exercise for people with heart disease. I tagged the UH Drusinsky Sports Medicine Institute to let them know that I had just met Dr. Lander, and I shared the article again. I also mentioned in the social media post that I would include this article in a future blog post.
I recommend reading the article, which follows:
Hypothesis 1 (Cardiac Condition) Rejected Again
August 14 & 28, 2024 - Hypothesis 5: Nerve Pain is the Cause of My Chest Pain
(Multiple Insults to my Chest Could Have Caused Nerve Damage)
[Wednesday, August 14, 2024, 10:30 am] Progress Notes Written by Harpreet Singh Chief Complain New Patient Visit (Chest pain ) . . . . . . Has been experiencing the symptoms for last 8 months or so. He denies any trauma or inciting event. He does report undergoing an open heart surgery for hypertrophic obstructive cardiomyopathy surgery was done early last year. Since the start of his symptoms he has an extensive cardiac workup and has seen 2 cardiologist who have ruled out any cardiac origin of his pain. He had stress test where his pain reduced while he was running on the treadmill. He has been eval by Dr. Melinda Lawrence from pain management who did costosternal junction injection which did not provide him with any relief. . . . . . . Would also trial him on gabapentin. = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = [Wednesday, August 28, 2024 11:00 AM] Progress Notes Written by Harpreet Singh Virtual or Telephone Consent . . . Chief Complain Follow-up (Fuv for pain in 2/10 in chest. /Started Gabapentin and its not helping the pain/Patient states he feel drunk and unstable) . . . . . . The patient rates the pain at 4 on a scale from 0-10. The patient describes pain as aching, burning. The pain is worsened by no aggravating factors identified and is alleviated by nothing relieves the pain. Since the last visit the pain has stayed the same. . . . . . . Last visit he was started on gabapentin, currently taking 100 mg 3 times daily which has not had any significant effect on his pain so far. I would recommend gradually increasing the dose to 200 mg 3 times daily. For next 3 to 5 days he would take 100 milligrams in the morning, 100 mg in the afternoon and 200 mg at bedtime, followed by 100 mg in the morning, 200 mg in the afternoon and 200 mg at bedtime for next 3 to 5 days, followed by 200 mg 3 times daily. Also discussed biopsychosocial model of chronic pain with patient. Given resources further education.
There are two parts to this section about dealing with Hypothesis 5 -- medication and the mental component of controlling pain:
Gabapentin for Nerve Pain
On August 14, 2024, University Hospitals pain management department doctor, Dr. Harpreet Singh, gave me a very thorough exam. Dr. Singh suggested that "multiple insults to my chest" (most recently my April 27, 2023, open-heart surgery) could have made my nerves react with pain even after the physical damage had been repaired. He prescribed gabapentin (sold under the brand name Neurontin) for nerve pain. I then had a virtual follow-up appointment with him the next week, on August 28th. I followed instructions to increase the dosage, starting on August 14th until the end of the month, at which time I started to decrease the medication, since I decided on a different course of treatment (see the surgery recommendation in the next section of this blog post). My new plan was to be completely off the medication by the end of the first week of September.
If I had continued with the nerve pain medication treatment, or decided to try it again in the future, Dr. Singh said its effectiveness varies from person to person. He has patients start at a low dose, and he keeps increasing it to see if side effects and the pain go away. Most people take the medication for a few months until the pain is gone, and then taper off to see if pain comes back.
I found that the gabapentin made me feel at times intoxicated and unbalanced, but that side effect should have gone away as my body adjusted to the medication. I did briefly stop writing this blog post during the time I was on the medication, since it prevented me from being able to concentrate on writing.
I did not finish this treatment, and planned to return to this treatment if needed in the future.
UnlearnYourPain.com
Even before I had my appointment with Dr. Singh, I was interested in learning about the mental component of controlling pain. On July 27, 2024, I had read the following two popular press articles:
Pain and the Mind-Body Connection
Mind-body therapies can help you reframe awareness of pain, so you can learn to use your mind to control pain.
January 11, 2024, at 11:54 am. By Jake Panasevich, E-RYT - U.S. News & World Report L.P.
This article is based on reporting that features expert sources:
Ellen Langer, PhD
Langer is a professor of psychology at Harvard University and author of “The Mindful Body, Thinking Our Way to Chronic Health.” Langer published the landmark “counterclockwise” study in 1979.
Tom Walters, DPT, OCS
Walters is a physical therapist and author of “Rehab Science: How to Overcome Pain and Heal from Injury.” Navigating pain is both an exercise in therapy and physical movements.Six Steps to Rewire Your Brain and Master Pain
Learn how visualization creates new connections in the brain to manage pain.
Posted October 30, 2020. By Evan Parks Psy.D. - Pain Rehabilitation - Psychology Today
At our second, virtual meeting (August 28, 2024), I asked Dr. Singh that, since I was healthy and there was no indication of what was causing the pain, shouldn't I just be able to mentally ignore (suppress??) the pain? He suggested I look at the website of Howard Schubiner, MD: UnlearnYourPain.com. He also said that there are psychologists who are experts in this field, and that this issue happens more to people who are perfectionists.
I also mentioned how I was writing a journal (this blog post) about my experiences this year with chest pain, and he said that journaling is one of the techniques to help become more mentally aware of your pain as you work to lessen the pain.
I found several "Mind Body Videos" on the website very interesting, but after watching a video that reviewed Dr. Schubiner's book Unlearn Your Pain (4th edition), I did not think its process fit my situation. Also, its companion website by Dr. Schubiner - - FreedomFromChronicPain.com - - stated that it is not for "Clearly diagnosed nerve injury" which at this point I thought I might have as a potential diagnosis.
Here are a YouTube playlist and additional videos that I watched. I would highly recommend visiting the "Mind Body Videos" web page for more resources.
Here is an excellent review of the book Unlearn Your Pain (4th edition) -- watch the video to learn if the book would be useful to anyone you know:
Hypothesis 5 (Nerve Pain) Not Fully Tested
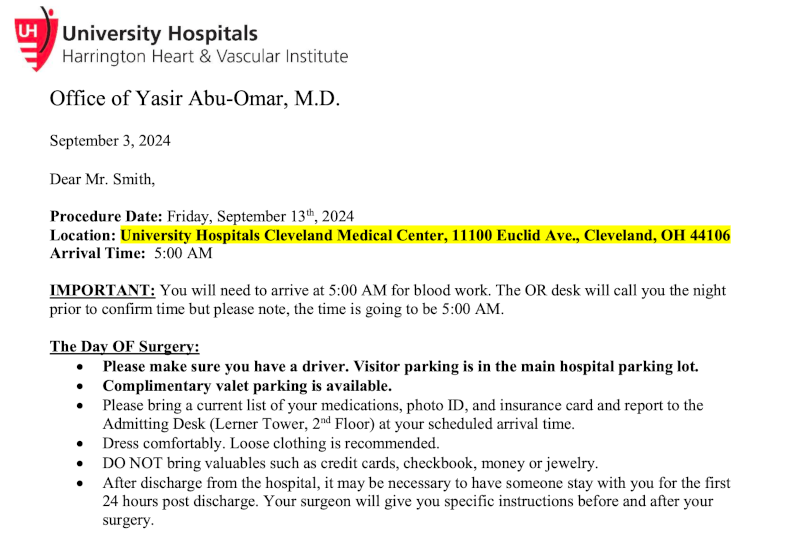
Friday, August 30, 2024 - Cardiac Surgery Clinic Appointment with Dr. Yasir Abu-Omar (Propose Testing New Hypothesis 6: My Chest Pain is Caused By Sternal Wires)
I had received a recommendation a while ago from a UH HCM Center nurse to update the cardiac surgeon who had performed my April 27, 2023, open-heart surgery, but I had still not done so. As I saw that I was entering the middle of the eighth month of 2024, I finally made the call. I thought it was just going to be a courtesy call to update the doctor about my chest pain, and an opportunity to again thank him for my successful 2023 surgery.
On August 13, 2024, I talked to my surgeon’s nurse so she could update my surgeon, Yasir Abu-Omar, MD. I figured that my pain chest issues treatment was not a surgery issue, but it would be good to just give him an update by telephone. Well, the same day, Dr. Abu-Omar’s secretary called back, saying that the doctor wanted to talk to me in person, and immediately scheduled an appointment for August 30, 2024.
As my appointment with Dr. Abu-Omar proceeded, I learned that my assumption about the appointment was completely wrong. I learned that while it is very rare, chest pain like mine can sometimes be caused by the sternal wires that were left in my body after the surgery. (To the right I added for a second time the same X-ray photo from April 4, 2024, that clearly shows the median sternal wires, and a close-up photo taken from the June 6, 2024, CAT Scan.)
The appointment ended with a recommendation to have the sternal wires in my chest surgically removed (the wires are no longer needed, since my sternum had healed a year ago), and a promise to receive a call the next workday (Tuesday, September 3rd) with a scheduled surgery date. I was told that it was a simple, short operation (that they could slip me in between other operations). I most likely would go home the same day, but was told to be prepared to stay overnight, if needed. I was also advised that the incision from re-opening the scar area of my chest should heal in approximately two weeks.
I was told that there was no certainty that the removal of the wires would get rid of my chronic chest pain, but the risks were low, and if it failed, I would continue with the several medication pain relief treatment options that Dr. Singh had already provided me.
At a future date, I hope to write the conclusion to this blog post: Hypothesis Proven: Chest Pain is Caused by Sternal Wires
[Friday August 30, 2024, 2:00 pm] Progress Notes Written by Yasir Abu-Omar I reviewed him at the clinic today. This gentleman underwent septal myectomy in April 2023. He had an excellent recovery with significant proved his and his symptoms. In December 2023 he developed nonspecific sharp chest pain. He has been under regular review with the cardiology team and has been seen by pain specialist. Several interventions were tried including lidocaine patches and most recently gabapentin with little help. On examination his wound appears to have healed well. Scar was somewhat hypertrophic. The sternum is completely stable. . . . presents with atypical likely musculoskeletal pain. I discussed with him the option of removal of the sternal wires in an attempt to ameliorate the pain. I told him there is no guarantee that this will work but it is worth a try. We discussed the risks and benefits and he is happy to proceed. I will schedule him in the very near future to be admitted hopefully as a day case for removal of sternal wires. Yasir Abu-Omar, MD
I ended the month of August 2024 looking at the following sternal wire removal resources:
Delayed chest wall pain due to sternal wire sutures
Ann Thorac Surg. 1991 Jan;51(1):56-9. doi: 10.1016/0003-4975(91)90448-y.
C E Eastridge 1 , S S Mahfood, W A Walker, F H Cole Jr
Published on the National Institutes of Health (NIH)'s National Library of Medicine websiteHypersensitivity reaction to sternal wires: a possible cause of persistent postoperative pain
Cardiovasc Surg. 1993 Aug;1(4):439-41.
N Ancalmo 1 , C Perniciaro, J Ochsner
Published on the National Institutes of Health (NIH)'s National Library of Medicine websiteThe outcome of sternal wire removal on persistent anterior chest wall pain after median sternotomy
Eur J Cardiothorac Surg. 2006 Jun;29(6):920-4. doi: 10.1016/j.ejcts.2006.02.013. Epub 2006 May 3.
Martin Agge Nørgaard 1 , Torben Colberg Andersen, Michael Jarner Lavrsen, Sven Borgeskov
Published on the National Institutes of Health (NIH)'s National Library of Medicine websiteYouTube video: Sternal wire removal
Feb 19, 2018. Dr Sudhir B V
Notice: Age-restricted video (based on Community Guidelines)
(NOTE: I think many people will not want to watch this graphic video, but I chose to watch it and share it here -- you have been warned. Plus, I am not sure that my procedure will look like this 2018 video.)
(NOTE: this next video features Dr. Lemaire -- I have two more excellent videos from his Cardiac Surgery Patient Education series in my second HCM blog post that explain open-heart surgery. Dr. Lemaire's videos and others that explain the process of how the sternal wires were placed in my chest can be found in the "Open Heart Surgery" videos section of my blog post: My Hypertrophic Cardiomyopathy Part Two: Surgery)
Sternum Wires & Heart Surgery: How Do Wires Work? Can I Get An MRI? What About Sternal Wire Removal?
I recommend viewing the following three chapters in this video I set the following links to open in a new window, and then play this video on the YouTube website:
Chapter 5) 2:59 How do sternum wires work
Chapter 7) 8:17 Can sternum wires be removed
Chapter 8) 9:35 How to remove sternum wires
Next - Testing Hypothesis 6: My Chest Pain is Caused By Sternal Wires!!
The end for now!
I promised myself when I started writing the draft for this HCM blog post on August 18, 2024, that I would stop writing at the end of the month. It is now the evening of Tuesday, September 3, 2024. (I gave myself three extra days to make up for the time I spent getting used to the gabapentin, which prevented me from writing.) I really am looking forward to the future date when I will finish this blog post with good news.
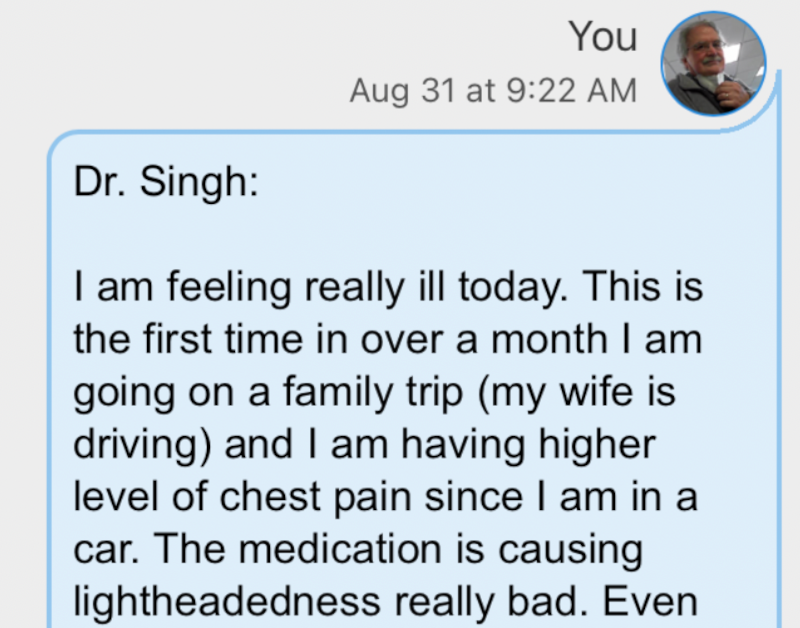
The past two months, I have missed all but two of the many events that I would normally attend in July and August, and canceled a big, once-in-a-lifetime trip that I had been planning for months. I was ill while at the two events I did attend, and wrote the following to two of my doctors:
[Saturday, August 31, 2024] I am feeling really ill today. This is the first time in over a month I am going on a family trip (my wife is driving) and I am having higher level of chest pain since I am in a car. . . .
To repeat how I started this blog post, the following reiterates the most important purpose of this blog post:
[I decided to write this blog post] to most importantly have a positive outlook for the future. Notice that the title includes the word "Recovery" at a time when there is no guarantee that I will get better. My plan is to write about what is happening to me through the end of August 2024, and then later add what the final outcome which I expect to be positive!
Yes, "I expect it to be positive!" I will achieve recovery, through either the now-planned surgery, or some medication, or taking control of pain with my mind, or something that I can't even imagine. I am already planning for when my life returns to my normal.
Tonight, I leave you with the next step that was confirmed by a call I received this morning (September 3, 2024), stating that my sternal wire removal surgery would be on Friday the 13th.
Note that the surgery was moved to Ahuja Medical Center, and I went home the same day.
PART TWO: Recovery Again
After writing everything above this point before Tuesday, September 3, 2024, I wrote the following on Monday, December 15, 2025, as I prepare for the end of the year on these last 16 days of 2025. It has been one full year and three months since my Friday, September 13, 2024, surgery to have the sternal wires removed.
SUCCESS!!
Hypothesis 6 (My Chest Pain is Caused By Sternal Wires) was supported by the evidence of how I was feeling in October 2024 and beyond!!!
After the surgery, the chest pain that seemed to come and go randomly was gone! For five months after the surgery, I very rarely experienced chest pain when I was fatigued, but never experienced pain without cause. For example, driving home from the Saturday, October 5, 2024, NASA International Space Apps Challenge (see my blog post about the event), I felt chest discomfort. The pain specialist had taught me that our bodies get used to being in pain, so after having months of worsening chest pain, it is to be expected that I have chest pain when fatigued or stressed. Chest pain reacting to stress is totally different to the random chest pain I was having before surgery. I am happy to report that the even this type of chest pain has completely gone away since Saturday, February 22, 2025.
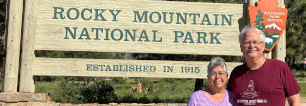
Recovery -- What recovery has meant to me now in 2025 is that I am back to my normal, active lifestyle, which in 2025 included two month-long backpacking trips (Allegheny Trail and Appalachian Trail) and active vacation trips with my wife. See photos from these trips in my two 2025 travel blog posts:
- Blog Date: September 16, 2025 - Colorado 2025: Rocky Mountain National Park, Estes Park, and Denver
- Blog Date: September 23, 2025 - Exploring New Hampshire, Vermont, and the USS Enterprise!

As I write this at the halfway point of December 2025, I am already planning some big trips for 2026. I will publish this blog post on December 31, 2025, as my way of celebrating the end of the year feeling that I am fully recovered -- back to my normal life -- just as I planned.
Here are the blog posts about activities I have attended since my Friday, September 13, 2024, surgery. I share them here to show what sort of activities I am able to do with no pain, and also to thank the organizers of these events. Please take a moment and scroll across the images/links below, and please click to read some of the 31 blog posts:
Related Blog Posts
We always like to include a list of related blog posts that may be of interest to the readers of this blog post, so here are my first three HCM treatment "Hypertrophic Cardiomyopathy" blog posts:
Blog Date: June 11, 2023 - My Hypertrophic Cardiomyopathy Part One: Diagnosis & Medication
Blog Date: June 11, 2023 - My Hypertrophic Cardiomyopathy Part Two: Surgery
Blog Date: June 11, 2023 - My Hypertrophic Cardiomyopathy Part Three: Hospital & Home
Here are my three recovery "Hypertrophic Cardiomyopathy" blog posts:
Blog Date: December 28, 2023 - My HCM Part Four: Recovery & A.T. Hike Featured on WKYC TV-3
"It was interesting to learn from his part of the interview that my cardiologist, Dr. Eiran Gorodeski, was not sure I would be able to backpack again. I plan to do even more backpacking in 2024."Blog Date: February 28, 2024 - University Hospitals Guest Post: HCM Patient Returns to Hiking the Appalachian Trail
I was asked to have my recovery story added to the Heart & Vascular Patient Stories sections of the University Hospitals website for February 2024 -- American Heart Month.